I have made extensive use of the knowledge I learned at The Dartmouth Institute in healthcare administration, healthcare economics, and health services research methods."
TARUN JELLA MPH'19
 Tarun Jella is researching the geographic and demographic characteristics of the U.S. medical and surgical workforce in the context of COVID-19 burden.
Tarun Jella is researching the geographic and demographic characteristics of the U.S. medical and surgical workforce in the context of COVID-19 burden.
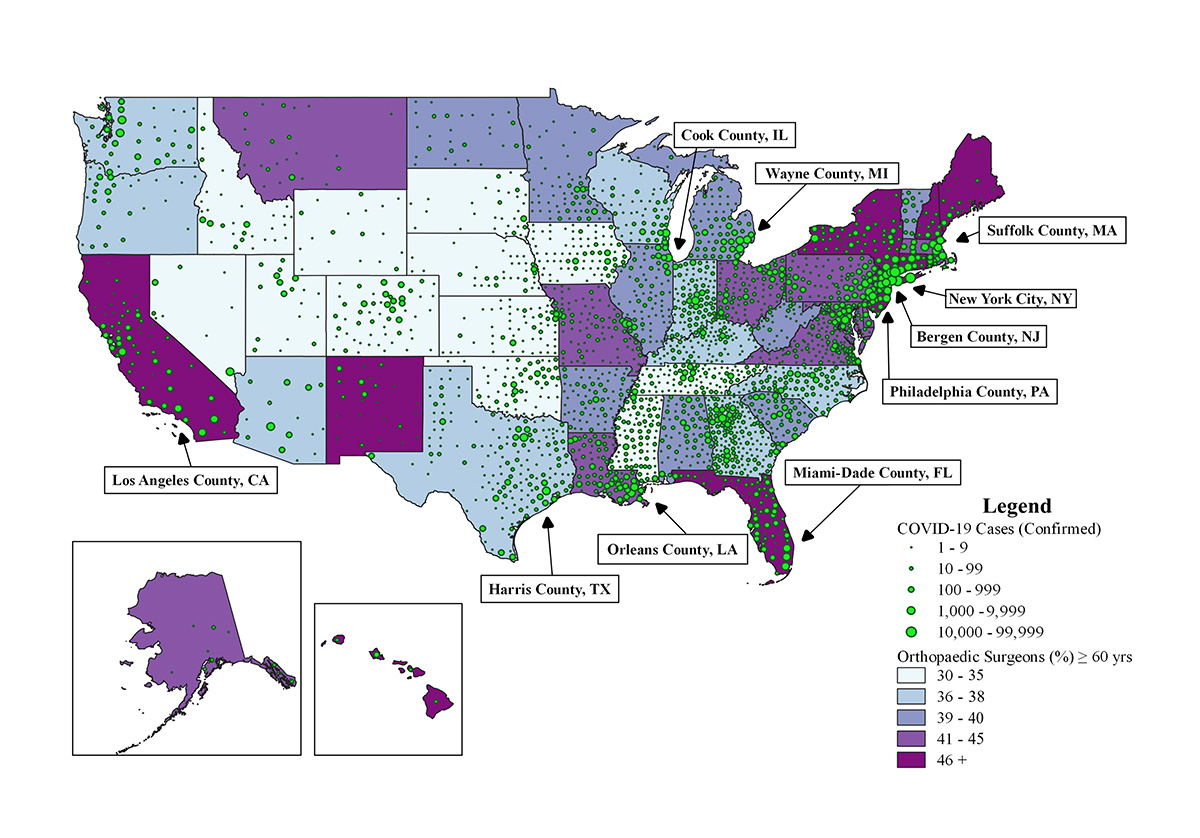
According to a new study Jella led in The Journal of Bone and Joint Surgery, four of the U.S. states with the highest quintile of orthopaedic surgeons aged 60 or older are also the ones most severely affected by COVID-19: New York, New Jersey, California, and Florida. (See a larger version of the geospatial map provided above). The findings prompt discussion about whether the situation may increase older surgeons' susceptibility to contracting the coronavirus as they continue to provide acute care and are recruited to the front lines of COVID-19 care.
A first-year student at Case Western Reserve’s School of Medicine, Jella has also been researching the economic and social impact of COVID-19 in terms of lost revenues to safety-net and public hospitals. Additionally, he is assessing the correlation between underlying racial disparities in Medicare population and death rates from COVID-19 among major U.S. cities.
.
My training from the MPH program has allowed me to approach my COVID-19 work with a passionate, empathetic, and system-level lens."
DANIELLE VOKE MPH'20
Danielle Voke is supporting the COVID-19 response through two roles. The first is working as a COVID-19 contact tracer with the Massachusetts Department of Health and Partners in Health to work with COVID-19 patients and help identify other individuals with whom they were in close contact.
In addition, Voke is interning with the Levy Serious Illness Health Care Delivery Incubator program at Dartmouth and Dartmouth-Hitchcock. The Incubator program focuses on developing and testing innovative healthcare delivery interventions to improve the quality of care for those with serious illness. Voke's internship work is centered on aggregating and reporting ongoing patient-centered COVID-19 innovations for the critically ill.
Voke says she appreciates the opportunity to apply skills she has developed in risk communication, patient-centered health communication, and healthcare improvement to both of her roles.
.
Armed with a greater understanding of public health concepts and approaches from The Dartmouth Institute, my training has helped me to guide, support, prioritize, and operationalize the many activities that we've been involved in."
MARY EVANOFSKI OT, MPH'11
 Mary Evanofski's COVID-19 work is two pronged at the Dartmouth-Hitchcock Medical Center in New Hampshire. There she serves as an Incident Command Planning Chief and Staffing Coordinator where she has played a critical role in organizational decision making and coordination of activities in response to COVID-19 from the beginning.
Mary Evanofski's COVID-19 work is two pronged at the Dartmouth-Hitchcock Medical Center in New Hampshire. There she serves as an Incident Command Planning Chief and Staffing Coordinator where she has played a critical role in organizational decision making and coordination of activities in response to COVID-19 from the beginning.
Some of the work that she is most proud of is establishing the "Staff Match" program. Staff Match is designed to place hospital staff, whose work functions had been reduced due to the pandemic, to jobs created by Dartmouth-Hitchcock's COVID-19 response. These jobs include a public-facing hotline, occupational medicine phone support and infectious disease testing triage, door screeners, supply chain assistance, runners, and PPE cleaners.
Evanofski is also the vice president of operations for the population health management division. The division has overseen the ramp up to using telehealth in primary care and psychiatry, as well as community efforts to provide food, transportation, and child care connections to those in need during the crisis.
TACKLING THE CHALLENGES OF COVID-19
During this unprecedented crisis, Dartmouth Institute students and alumni are impassioned more than ever to improve the health of their communities.

